Breast Cancer Vaccine Shows Promise as it Enters Phase 2 Trial
About 20% of breast cancers exhibit elevated levels of a protein known as HER2. You may have heard the classifier “HER2-positive” breast cancer, which refers to these cases. HER2 status remains a paradoxical factor in breast cancer diagnosis. While HER2-positive cancer cells grow quickly and aggressively, HER2 can also serve as a therapeutic target, increasing the likelihood of a HER2-positive breast cancer patient responding to treatment.
A monoclonal antibody called trastuzumab remains highly effective in treating HER2-positive breast cancer patients. When trastuzumab binds to HER2 on cancer cells, it inhibits cell growth. Some patients successfully treated with trastuzumab develop HER2-specific immunity, which confers a favorable prognosis, including extended progression-free and overall survival. Studies have demonstrated that HER2-specific T cells also play a role in protecting patients from breast cancer recurrence.
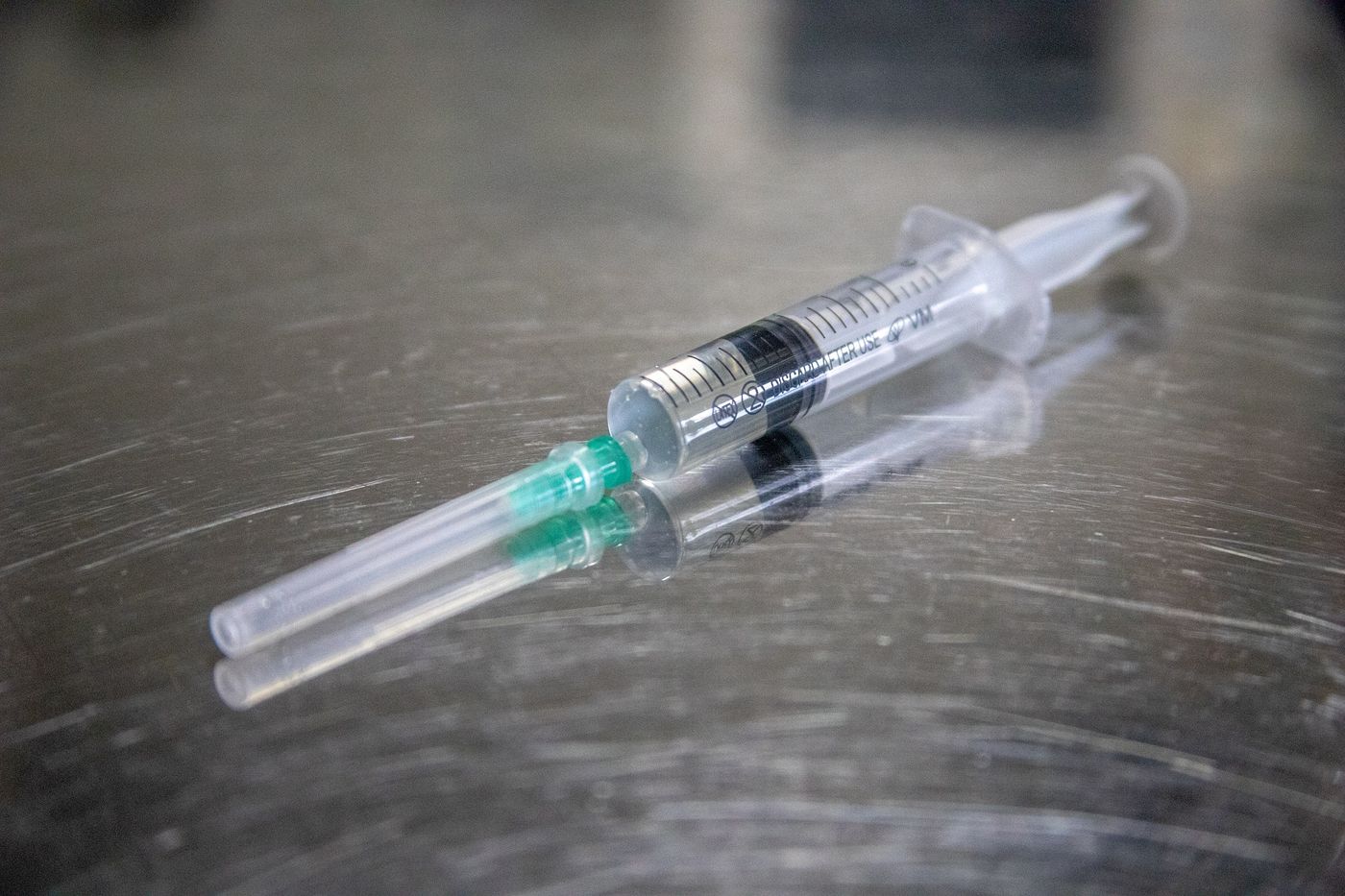
Unfortunately, trastuzumab does not induce HER2-specific immunity in all patients. To develop a method to increase the number of breast cancer patients developing beneficial HER2-specific immunity, and the accompanying good prognosis, a team of researchers investigated the efficacy of a plasmid DNA vaccine encoding for part of the HER2 protein. The researchers recently published their findings in JAMA Oncology.
The investigators carried out a phase 1 clinical trial (NCT00436254) to assess potential toxicities associated with vaccination. The study included 66 patients diagnosed with stage III or IV HER2-positive breast cancer, and the researchers compared three doses of DNA vaccine (22 patients received each dose). In addition to evaluating for toxicity, the investigators measured immunity associated with vaccine treatment by examining the immune cells circulating in the blood.
Patients received three doses of the vaccine along with an adjuvant called granulocyte-macrophage colony-stimulating factor (GMCSF). The investigators observed no severe toxicities associated with treatment. Participants most often reported injection site reactions (82%) as an adverse event, but smaller percentages of patients experienced flulike symptoms (33%) and fatigue (36%). Notably, the study included ten years of follow-up, so the researchers ruled out long-term adverse events associated with the vaccine.
When measuring measured HER2-specific immunity, the researchers found that higher doses of vaccine demonstrated better immune responses than the patients receiving the lowest dose. The authors conclude that their findings demonstrate that this HER2 DNA vaccine induces immunity. The research team has begun a phase 2 randomized clinical trial (NCT05163223).
Sources: Cancer Res, JAMA Oncol (Datta), JAMA Oncol (Disis)