Worst COVID-19 Cases May be Caused by Immune Cell Overactivity
Right now, we can't be sure of exactly how many people have been infected by the pandemic virus SARS-CoV-2, but we know the virus can cause a wide range of symptoms, and infections may be asymptomatic in many people. When it causes an illness, COVID-19, it's a respiratory disease characterized by sore throat, fever, and the loss of the ability to smell. If a case gets worse, the infection starts to interfere with a person's ability to breathe, and it may eventually result in death. Researchers have now found that in some of the worst cases of COVID-19, overactive immune cells may be responsible.
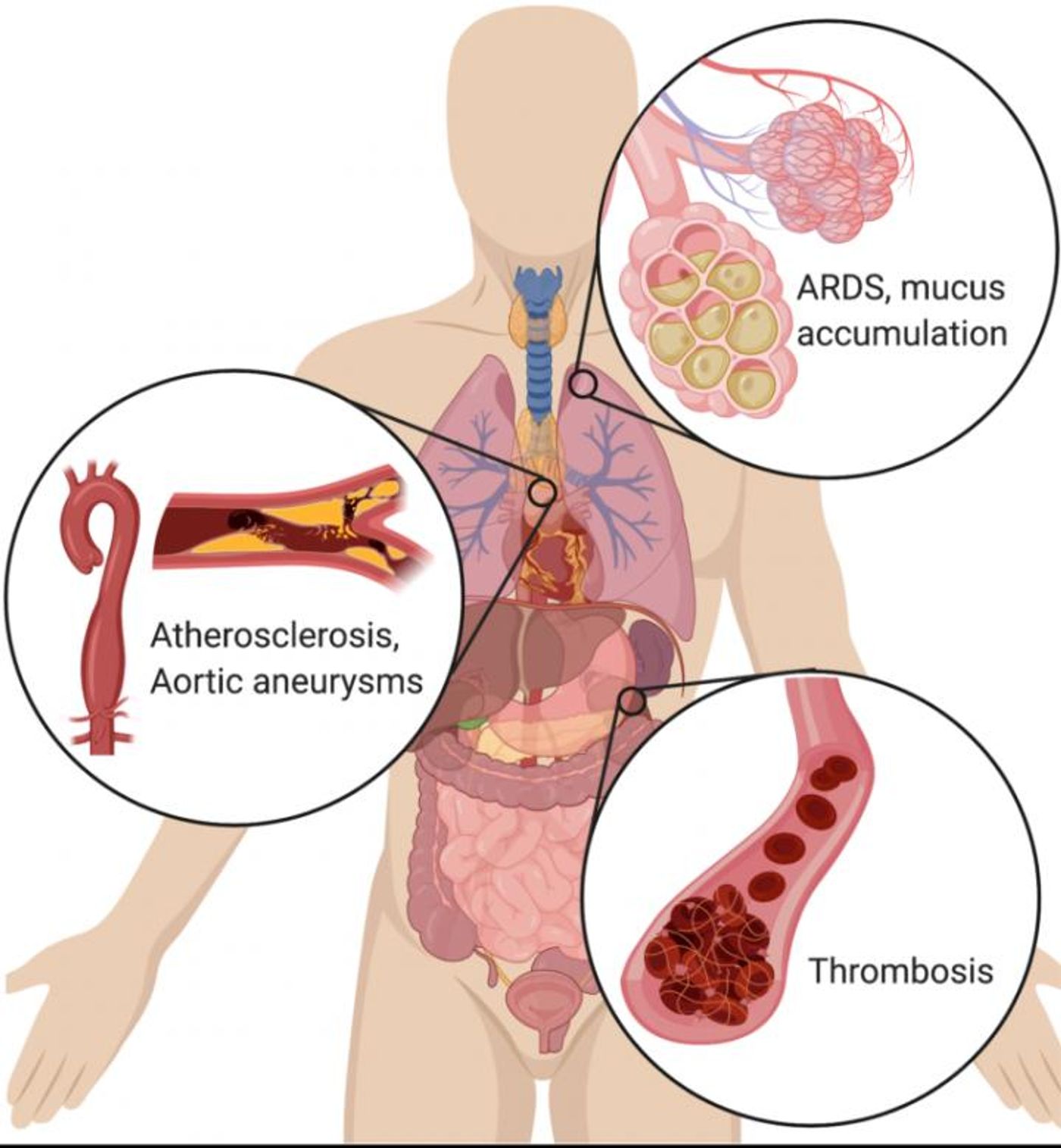
In COVID-19, the airways are affected because the virus attaches to receptors that are found on the surface of respiratory cells; it gains entry into those cells, causing infection, inflammation, and the production and release of more viral particles. Other than breathing difficulties, the worst cases are also characterized by thick mucus in the airways, lung damage, blood clots, and Acute Respiratory Distress Syndrome (ARDS), which is when a ventilator is often applied to force air into the lungs. A large proportion of people that are affected in this way will end up dying.
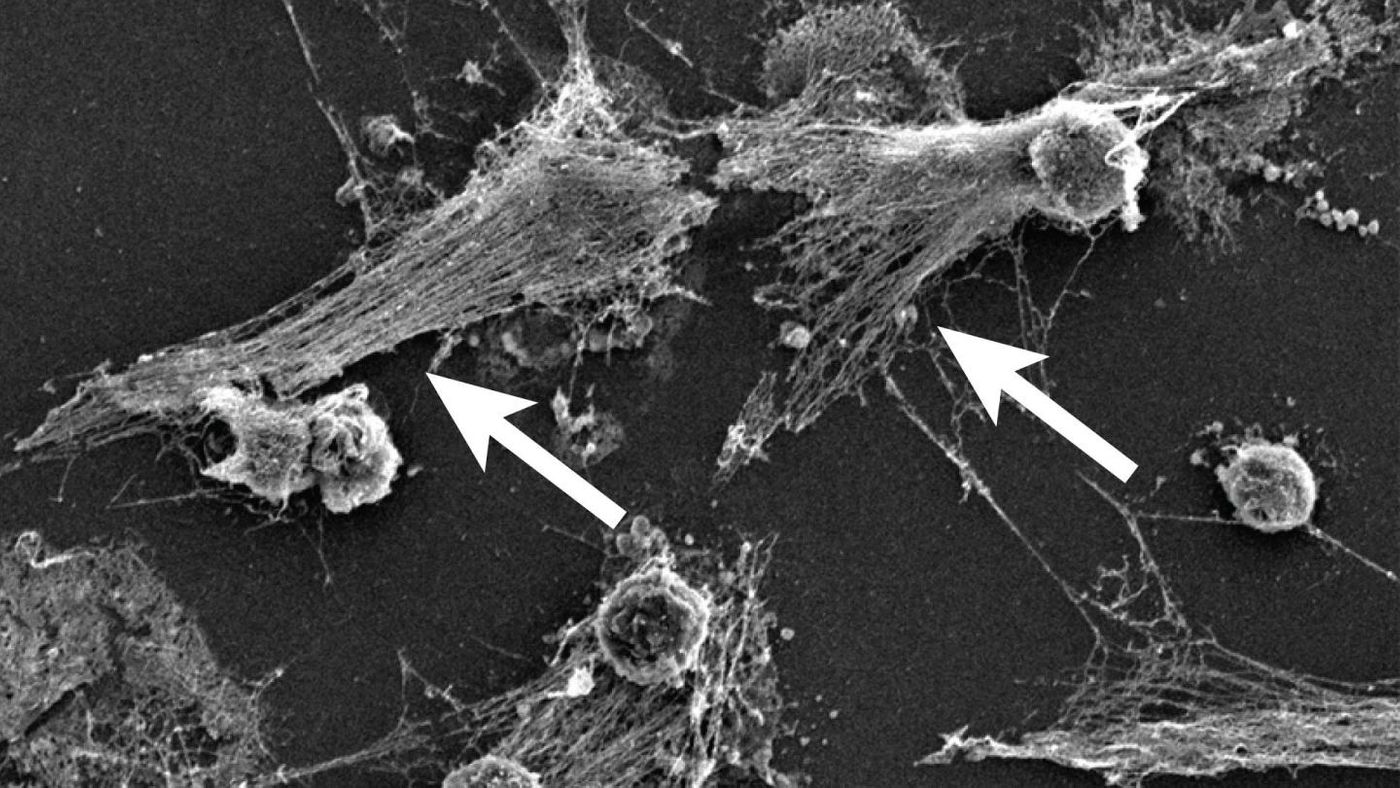
Now, a research consortium called the NETwork has suggested that these severe cases are caused by overactive neutrophils, which are immune cells that identify bacteria and destroy them with neutrophil extracellular traps (NETs). NETs are a mixture of DNA and toxic enzymes and the dysregulation of their acitivty is suspected to play a role in some autoimmune disorders. While they serve a critical purpose in most cases, they may also be generating an overwhelming response to COVID-19, one which damages the lungs and other organs.
"Given the clear similarities between the clinical presentation of severe COVID-19 and other known diseases driven by NETs, such as ARDS, we propose that excess NETs may play a major role in the disease," said the co-corresponding study Betsy Barnes, Ph.D., professor at the Feinstein Institutes. "As samples from patients become available, it will be important to determine whether the presence of NETs associates with disease severity and/or particular clinical characteristics of COVID-19."
"NETs were identified in 2004, but many scientists have never heard of them. Most of the researchers in the NETwork have worked on NETs in other diseases, and when we started hearing about the symptoms of the COVID-19 patients, it sounded familiar," noted the senior study author and Cold Spring Harbor Laboratory cancer biologist Mikala Egeblad, Ph.D.
Clinician scientist Jonathan Spicer, M.D., Ph.D., is an Assistant Professor of Surgery at McGill University and a thoracic surgeon who has treated severe COVID-19 cases. "We see in these patients severe lung damage known as ARDS, another serious problem caused by excess NETs and seen in cases of severe influenza," he said. "In addition, their airways are often clogged with thick mucus and unlike most severe lung infections, these patients tend to form small clots throughout their body at much higher rates than normal. NETs have also been found in the blood of patients with sepsis or cancer, where they can facilitate the formation of such blood clots."
The researchers are now working to determine how often NETs factor into COVID-19 cases. If they confirm that NETs are responsible for the worst symptoms, treatments that target them might be considered as an option for COVID-19 patients. This approach may help reduce the need for ventilators.
Sources: AAAS/Eurekalert! via Cold Spring Harbor Laboratory, Journal of Experimental Medicine