Exosome delivery of an anti-HIV drug to the brain
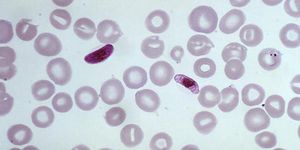
The body has a remarkable ability to prevent foreign objects, such as toxins or other pathogens, from entering the brain. This is accomplished through several mechanisms such as metabolizing these foreign objects in the blood stream before they reach the brain. Another notable way the body protects the brain is through a physical barrier, composed of blood vessels with unique properties that regulate the movement of nutrients, cells, and molecules between the blood and the brain. This barrier, called the blood-brain barrier, is critical for keeping the brain safe, but conversely can also prevent lifesaving drugs from reaching the brain. Recently, researchers from the City of Hope developed a new drug delivery system that can easily bypass the blood-brain barrier and deliver an anti-HIV drug to the brain.
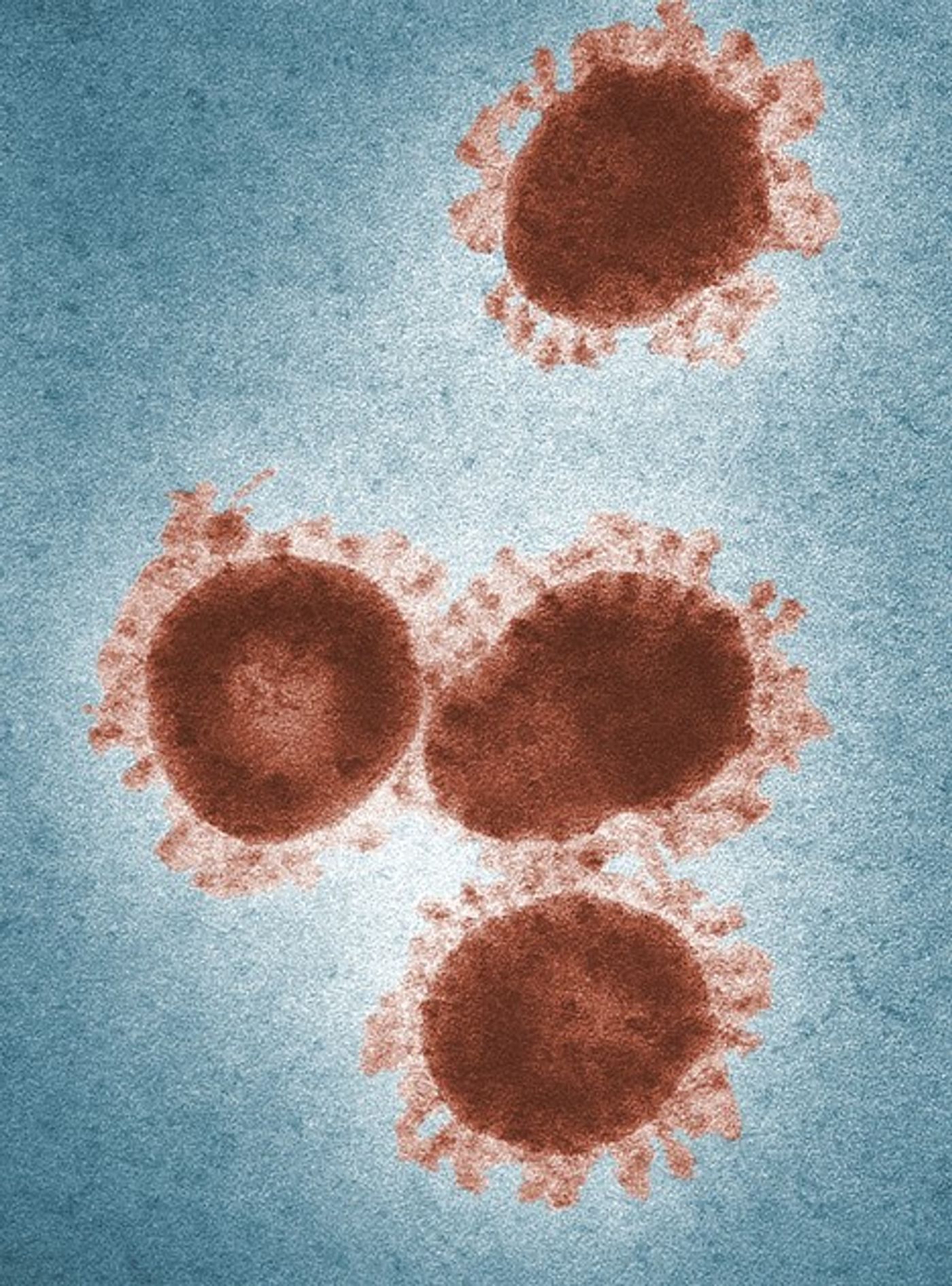
In research published in the journal Nature Communications last week, investigators engineered nanosized exosomes to deliver their anti-HIV drug. Exosomes can best be described as small vesicles that are normally released by cells for a variety of purposes, like cell-to-cell communication. In the study, the researchers packaged the engineered exosomes with an anti-HIV protein drug called ZPAMt HIV protein repressor. The exosomes were then systemically administered to mice that expressed the HIV virus, and the researchers then looked at the brains, bone marrow, and spleens of these mice. They found that 10 weeks after treating the mice with the ZPAMt exosomes, there was a significant suppression of HIV in all tissue including the brain. Additionally, because of the design of the drug, it was able to block the ability of HIV to replicate and lock it in a dormant state, in a mechanism referred to as “block and lock.”
This study is remarkable because it shows that the engineered exosomes can effectively cross the blood-brain barrier to deliver a drug payload to the brain. Furthermore, this study is important for HIV treatment research because the ZPAMt drug was shown to effectively block and lock HIV in brain tissue. A senior author on the study, Kevin Morris, PhD, said, “This is the first time that block and lock has been successfully delivered to treat HIV in vivo in the brain.” HIV affects approximately 1.2 million people in the United States and there is currently no cure for the disease. However, this research provides a way forward for an effective new treatment to lessen the burden of the disease.
Sources: Nature; BMC Biology; CDC