Transforming T Cells into Powerful Memory Cells That Target Cancer
New cancer treatments are now based on harnessing the power of the human body’s own immune cells to get the job done. The job? Specifically target cells overcome with cancer, eliminate them, and prevent cancer from spreading to more cells, tissues, and organs. A new cellular therapy follows such an approach, utilizing the power of T cell conversion to target cancer.
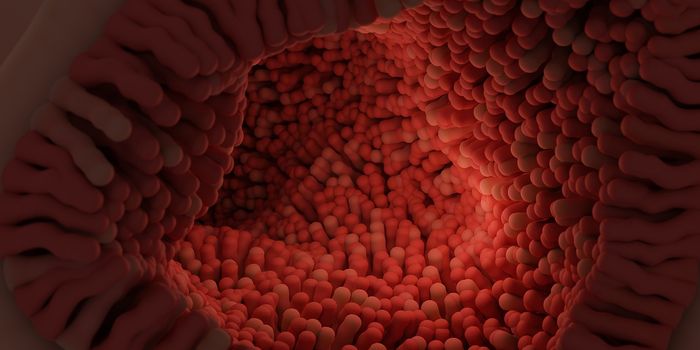
Cellular therapies are used to target cancer, and the science behind these therapies is based on identifying specific T cells, extracting them from the host, treating them in the lab, expanding the cells in the lab, and returning them to the host for a desired, anti-cancer effect. The specific T cell type that results from such therapies is usually effector CD8-positive T cells. A successful cellular therapy will create such T cells fully equipped to target specific tumor cells based on cell-surface antigens.
The new therapy’s main goal is to transform effector T cells into a strong hive of memory T cells. Why memory T cells? This population of immune cells has a proclivity toward growth. They are durable and “capable of self-renewal.” They are also able to trigger the targeting of cells for destruction, such as cancerous cells.
“What they see, they kill very well,” explained senior author Cassian Yee, MD.
Yee’s team is also focused on supporting memory T cell growth because this cell type is persistent, and without a tenacious population of T cells, cellular therapies often do not achieve success.
After identifying and extracting T cells from a host, Yee’s team treated the cells with a combination of:
- An epigenetic drug, panobinostat
- A cytokine, interleukin (IL)-21
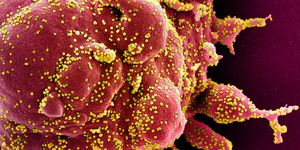
IL-21 activates STAT3, a protein required for the interaction between T cell stimulatory protein CD28 and its genetic promoter region. Without the IL-21 treatment, histone proteins inhibit this interaction, preventing CD28 activation. CD28 is a protein expressed on the surface of T cells that plays an important role in T cell activation and survival.
Before Yee’s team treated extracted T cells with panobinostat, they used a different drug called vorinostat. However, pabinostat is less toxic and more effective at producing memory T cells. In addition to the treatment, researchers expanded the T cell populations in the lab.
Yee’s team’s work on the new cellular therapy joins a group of similar therapies that rely on expanding T cells in the lab before returning them to the host:
- Chimeric antigen receptor T cells genetically modified to attack a specific target and used to treat B cell blood cancers
- Leukocytes extracted from tumors to treat melanoma
- Endogenous T cells transformed into super powered T cells equipped to attack tumor cells in the blood
Sources: University of Texas M.D. Anderson Cancer Center, Cancer Immunology Research, Immunity