An Improved Understanding of 'Original Antigenic Sin'
"Original antigenic sin" is a phenomenon that was identified in 1960; it refers to a hypothesis about the physiology of the immune system. In orignal antigenic sin (OAS), the immune system opts to rely on the memory of an infection when it is exposed to a similar, but not identical pathogen rather than mounting a novel response to the new pathogen. This could lead to an inadequate reaction to the new pathogen, because instead of adapting to efficiently eliminate the new infection, the immune system sticks to its immunological memory of the old infection. The immune system may become 'biased' to the memory, continually producing old antibodies against a virus it no longer encounters. OAS might influence our response to vaccines. But don't give up your booster shots just yet, because there is a twist.
Researchers have learned more about when OAS occurs, which can help scientists improve the effectiveness of vaccines and boosters. The findings have been reported in Nature.
"Our goal was to understand the basic principles that underlie OAS so that researchers making these vaccines can keep the potential effects in mind," said senior study author Gabriel D. Victora of Rockefeller University. "With a novel technique, we lay out the basics of how OAS should be looked at from an experimental perspective and answer a question we believe to be key to vaccine development."
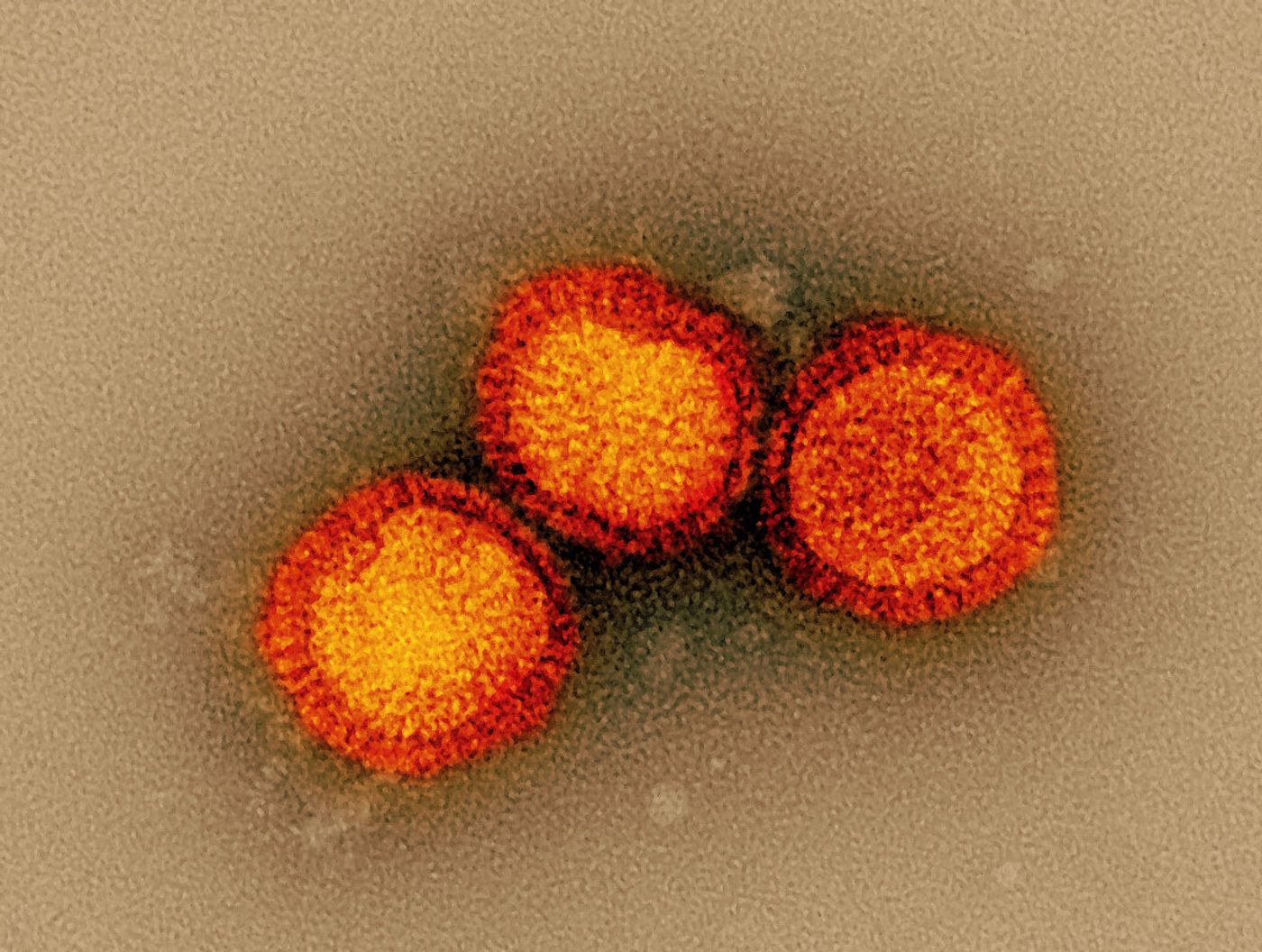
OAS could make it difficult for the immune system to respond to new flu strains, even when individuals get the seasonal flu vaccine. If OAS occurs, the B cells that were first exposed to influenza would keep producing antibodies against that strain, suppressing the creation of new ones.
"According to the OAS idea, your body wouldn't be able to develop new immune responses to evolving variants of a virus, because it would be addicted to the first strain you encountered," said Victora.
OAS is challenging to assess the laboratory, however. Sometimes it's been identified in experiments, while other researchers have not been able to reproduce those findings. In this study, the researchers developed a protocol to distinguish between old and new antibodies that were circulating in mouse serum. The mice were then repeatedly immunized, and the investigators tracked each antibody.
This effort revealed that when antigens that stimulate immunity remained the same, the mouse immune system continued to rely on the first B cells that were made in response to that antigen, and new B cells were not made. The researchers estimated that these mice would have otherwise made 55 times as many new antibodies if those old antibodies were not lingering around, preventing the formation of new antibodies, said Victora.
These findings make it seem like booster shots are useless, because the immune system will keep going back to those old B cells. But that is not always the case.
When booster shots contain antigens that differ, even only a bit from the original antigen, the OAS phenomenon does not occur. When mice were exposed to various strains of infleunza and SARS-CoV-2 that differed by a few amino acids, the B cell deficit was dramatically restored from a 55-fold loss to a 3-fold loss, which would be manageable.
"When boosting with a variant antigen, we begin to see new, variant-specific antibodies that enable the subversion of OAS," said first study author Ariën Schiepers, a graduate student in Victora's lab. "This work...underscores the ingenuity and adaptability of the immune system."
This research has also not yet been confirmed in humans. A wealth of human data has shown that seasonal flu shots, which are often very different from the previous years' shots, effectively reduce illness. Some research has suggested that repeated flu shots may slightly blunt their effectiveness, but a meta-analysis showed that it was still best for people to get the flu shot. Those findings have also been confirmed for COVID-19 vaccines; individuals who have received a full vaccine series and booster shot were far less likely to have a severe infection that requires hospitalization compared to people who had not been vaccinated or only got one dose.
Sources: Rockefeller University, Nature