New research has suggested that after long-term follow-up, HIV is no longer detectable in a patient that was previously HIV-positive. Only certain people will qualify for the high-risk treatment that the patient received, but this stem-cell transplant-based therapy has now been successful twice, showing that it's possible to cure HIV infections.
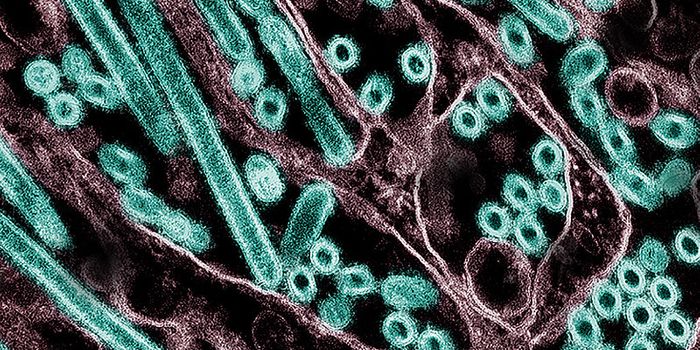
Reporting in The Lancet HIV, an HIV patient underwent stem cell transplantation, receiving cells from healthy donors that carry a genetic mutation that makes them resistant to HIV. While HIV-1 DNA has integrated into tissue samples taken from the patient, there was no active infection that could be detected 30 months after drugs that treat HIV infections called antiretroviral therapeutics were halted. The remnants of DNA in these tissues are thought to be unable to trigger viral replication.
"We propose that these results represent the second ever case of a patient to be cured of HIV. Our findings show that the success of stem cell transplantation as a cure for HIV, first reported nine years ago in the Berlin patient, can be replicated," said the lead study author Professor Ravindra Kumar Gupta of the University of Cambridge.
He cautioned, however, that this approach is "a last resort for patients with HIV who also have life-threatening hematological malignancies," and would not be useful for HIV patients that were being treated successfully with antiretrovirals. Current therapeutics enable most HIV-infected patients to live a healthy, long life. This work may help open up avenues to a cure that most patients can use, however.
The treatment involves totally irradiating the body, then transplanting stem cells from a donor that carries mutations in a gene called CCR5, which renders them impervious to HIV infections. The patient then undergoes a chemotherapy regimen. Both the irradiation and chemotherapy are meant to destroy residual virus, while the transplanted stem cells are supposed to prevent the virus from replicating anew.
This treatment was successful; the scientists showed that 99 percent of immune cells in the transplant recipient were derived from the donor. Only one transplant was needed for this patient; in the first case, the Berlin patient, there were two. The second, the London patient will also be monitored to check for the reemergence of the virus.
"Gene editing using the CCR5 has received a lot of attention recently. The London and Berlin patient are examples of using the CCR5 gene in curative therapies outside of gene editing. There are still many ethical and technical barriers - e.g. gene editing, efficiency, and robust safety data to overcome before any approach using CCR5 gene editing can be considered as a scalable cure strategy for HIV," noted study co-author Dr. Dimitra Peppa of the University of Oxford, UK.
Sources: AAAS/Eurekalert! via The Lancet, The Lancet HIV