Poor Oral Hygiene May Worsen Gut Inflammation
Good dental hygiene benefits more than just the teeth and gums; researchers have found that poor oral health can contribute to the development of diseases like heart disease and pneumonia. Now scientists have reported in Cell that an unhealthy mouth may also exacerbate the symptoms of bowel diseases including ulcerative colitis and Crohn's disease. These inflammatory conditions are thought to affect as many as three million Americans.
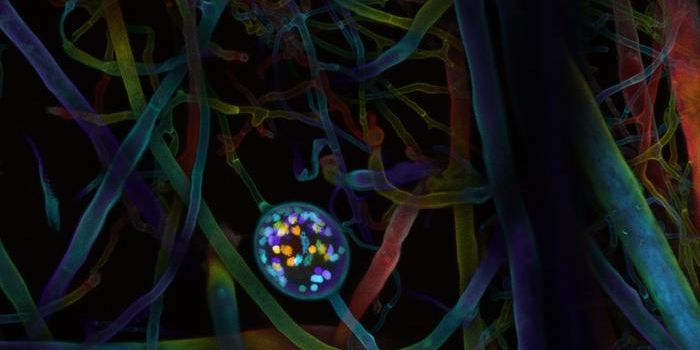
The human body is host to trillions of microbes, which live in and on us. This research studied how microbes that reside in the mouth, the oral microbiome, is connected to bowel disorders. Nobuhiko Kamada, Ph.D., assistant professor of internal medicine in the division of gastroenterology, has researched the gut microbiome for years. He has taken note of reports that have linked inflammatory bowel disease to the presence of oral microbes in the gut. "I decided to approach the dental school to ask the question, does oral disease affect the severity of gastrointestinal diseases?" said Kamada.
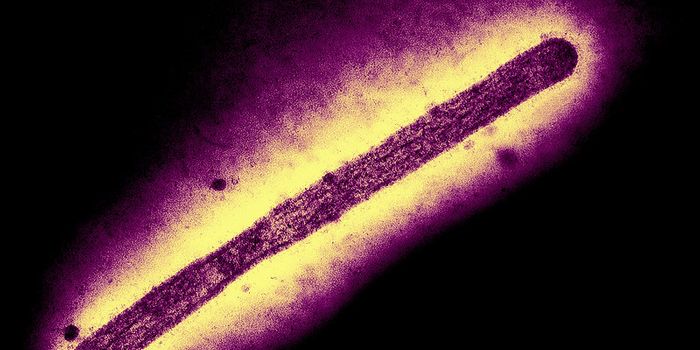
Periodontitis, or gum disease, is connected to imbalances in the oral microbiome. There is a rise in the levels of bacteria that cause inflammation, and these pathogenic microbes can then migrate to the gut.
While these oral microbes promote inflammation in the gut, they might not cause it directly. This research used a mouse model of colon inflammation to study the process. The findings suggested that these bacteria can make existing gut inflammation worse.
"The normal gut microbiome resists colonization by exogenous, or foreign, bacteria," said Kamada. "However, in mice with IBD, the healthy gut bacteria are disrupted, weakening their ability to resist disease-causing bacteria from the mouth." The researchers determined that when oral and gut inflammation was occurring in mice, their weight and disease symptoms were also rising.
The scientists also suggested that periodontitis can trigger the activity of immune cells, T cells, in the mouth, and these cells then move to the gut and make inflammation worse. Normally, the gut is capable of defending against invading bacteria while also ensuring that there is not an excess of inflammation. Since there are so many microbes in the gut, a careful balance must be maintained. Kamada explained that in the mouth, inflammation tends to produce inflammatory T cells that can make disease in the gut worse by triggering inflammation.
"This exacerbation of gut inflammation driven by oral organisms that migrate to the gut has important ramifications in emphasizing to patients the critical need to promote oral health as a part of total body health and wellbeing," said study co-author William Giannobile, DDS, the William K and Mary Anne Najjar professor of dentistry and chair of the department of periodontics and oral medicine at the U-M School of Dentistry.
"Far too many patients still fail medications, leading to reduced quality of life and eventual surgery," said study co-author Shrinivas Bishu, M.D., assistant professor of gastroenterology. "This study importantly implies that clinical outcomes in IBD may be improved by monitoring oral inflammation - an intriguing concept."
Sources: AAAS/Eurekalert! via Michigan Medicine - University of Michigan, Cell