What's the deal with SARS-CoV-2's spike protein?
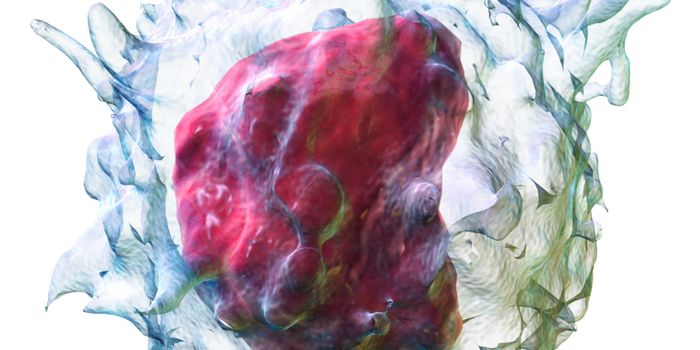
Structurally, SARS-CoV-2 (the viruses that cause COVID-19) are spherical shells made up of a lipid membrane, with a core containing the virus’ genetic material. This genetic information on its own is not enough for the virus to replicate. For this, it needs to first infect a living cell.
Intense vaccine development efforts are currently underway, with many programs focused on priming the immune system against a specific protein on the surface of SARS-CoV-2, known as the spike protein. These protein projections protruding from the surface of the virus give it a “crown-like” appearance and have been found to help it to infiltrate human cells.
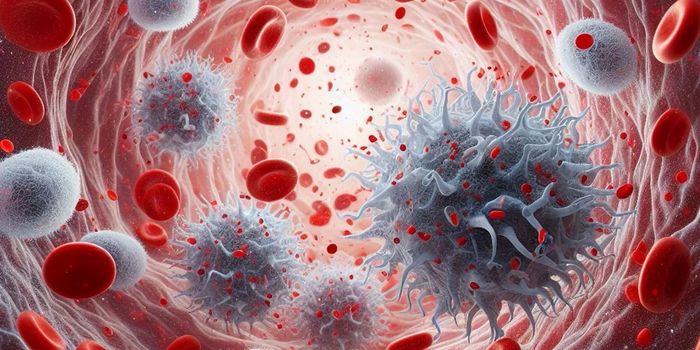
During infection, the spike protein acts as a key, binding to receptors on human cells in a process that is activated by enzymes present on the host cell. This enzyme-mediated process “unlocks” cells and allows the virus to gain entry, where it then hijacks the cell’s machinery to replicate.
Interestingly, while other coronaviruses also bear spike proteins, emerging genomic analysis has revealed some unique features of those present on SARS-CoV-2. Researchers have identified that COVID-19 infections occur as a result of spike proteins that have been activated by a particular host-cell enzyme called furin. Significantly, furin is not only present on lung cells, but also in the tissues of the liver and small intestine, giving SARS-CoV-2 multiple potential entry points into the human body. Scientists have attributed liver failure in some COVID-19 patients to this particular characteristic.
Other researchers believe that this special furin activation site could also affect the virus’ stability, pathogenicity and mode of transmission, enabling the rapid spread of infection between individuals.
However, when it comes to relating SARS-CoV-2’s distinctive spike protein to its infectivity, not all scientists see eye to eye. Researchers have not yet mapped the precise molecular pathways occurring during viral entry, nor do they fully understand how the virus’ activation sites correlate with its virulence. While comparing SARS-CoV-2's structural components to that of other SARS viruses may offer some clues, it remains challenging to draw solid conclusions. For example, the influenza virus, which does not have a furin activation site, was responsible for the deadliest recorded pandemic, the Spanish flu of 1918.
The receptor on human cells that the spike protein attaches to is called angiotensin-converting enzyme 2 (ACE2), with this attachment being facilitated by the spike protein's furin activation site. The binding of SARS-CoV-2 to this receptor is at least ten times stronger than that of other SARS viruses, which may be an important factor influencing COVID-19 transmission rates. As an alternative to vaccines that target the spike protein, scientists predict that other therapeutic strategies could also be effective, such as temporarily blocking ACE2 in cells to prevent the entry of the virus.
Presently, the SARS-CoV-2 spike protein is being heavily used as a target antigen in vaccine development. It serves as a unique molecular identifier that the immune system will “remember” to resist COVID-19 infection. At the same time, scientists like Gary Whittaker, a virologist at Cornell University, continue to delve into the intricacies around exactly how the spike protein infects human cells so well. By removing or modifying specific sites on the protein, the research team is studying how the protein’s sequence relates to viral infectivity. Understanding the spike protein’s role in the context of the COVID-19 pandemic is no easy feat, considering so much has yet to be discovered about the biology of this newly emerged virus. According to Whittaker, “Coronaviruses are unpredictable, and good hypotheses often turn out to be wrong.”
Sources: Nature, The Harvard Gazette.